What makes a good physical therapist?
I was thinking about this as we end 2018 here in Reno and begin focusing on 2019 for Nevada Physical Therapy. One of the things we are constantly trying to improve on is the Patient Experience. We want every patient to have an amazing experience here which may be an odd concept because we don’t sell churros and most of our patients are in pain when they come to see us. Yet, this is also the population that needs to have a positive experience the most. They are often depressed, anxious or scared that this injury will not get better; that they will be relegated to a life of pain which grants great responsibility on our profession and specifically, our clinicians. So it got me thinking, what makes a good physical therapist? Here’s what I came up with and true to point number 3, this is an ever-evolving list.
-
Empathy. Most of us got into this profession because we had been exposed to an injury at some point in our lives. The ability to relate to our patients cannot be overstated. Often times, if you come to see me, I may share a story about a similar injury I had and as I approach 40 years of age and am closing in on a decade of competing in powerlifting, I have several. I do this not because I’m not listening (see point 2), but because I want you to know that I can appreciate what you may be going through. I’ve been scared something won’t get better, I’ve doubted my ability to come back from an injury, and I’ve googled various maladies to the ends of the internets. A good physical therapist must be able to offer a rope out of the hole we often end up in and being empathetic to our patients’ unique pain experience is essential to develop trust, establish buy-in that you can actually help them, and create a therapeutic alliance.
-
Be an active listener. This doesn’t mean nodding dramatically with uninterrupted eye-contact as a patient recounts their journey into your clinic. It means truly listening to a person. This means, in part, trying to figure out the psychosocial contribution to a patient’s experience. What are their past experiences with pain? What are they afraid of and how can I address these fears in a way that makes sense to them? Additionally, it means not diagnosing them before they’ve finished their introduction which sounds intuitive but often, physical therapists can fall victim to wanting to point a finger at the patient’s “problem” so we can implement our favorite treatment system as quickly as possible and consequently may miss important details in the examination. A recent example, I had a patient come in with proximal (high) hamstring pain that had failed a classic Mckenzie approach to a disc injury at a different clinic. I love proximal hamstring tendinopathies because I think they are often misdiagnosed so it is an area where we often succeed where other clinics may not because we spend SO much time working on tendinopathy protocols. In my head, I’m working out her day 1 plan to minimize compression while we build load tolerance to the hamstring complex, et cetera et cetera, when she said something that pricked my ears: she felt better after pull-ups. Wait…that doesn’t add up. A little more digging and assessment and we established that her primary pain driver was lumbar extension, or specifically, compression to the nerve root. She’s well on her way to getting better but even experienced clinicians need to be hyper-vigilant to not let their biases jump the process.
-
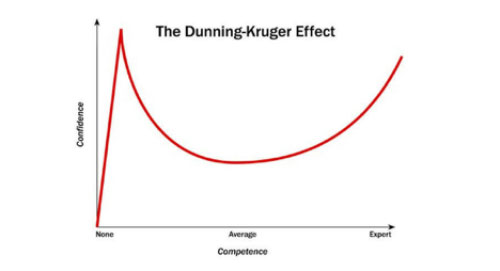
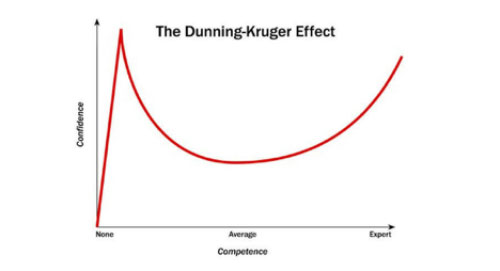
Being comfortable with uncertainty. We live in a weird time when social media followers and/or a high skill in an athletic task have been equated with knowledge and subsequently, trust. This is a challenging time for healthcare consumers being inundated with information; sold quick fixes and silver bullets for a variety of maladies so the question is…who’s right? The answer is not very straight forward but when in doubt, choose a clinician that is honest and uncertain. When you’ve spent a decade in this profession, you have the experience and time on your side to know that what you previously believed to be true may not be in line with the current best evidence and your belief system must be fluid. I honestly cringe when I remember some of the things I’ve told patients in the past that are now known to be inaccurate, unsubstantiated by the science, or just plain wrong. I do not dwell on these things as it is a natural part of professional development but instead use those examples as a reminder that what I may believe now is absolutely susceptible to change and evolve based on the literature. Instead of trying to be “more right”, I think a good clinician is aware that we really are trying to be “less wrong” when it comes to treating human beings. We are just scratching the surface of complicated topics such as pain science, non-specific low back pain, “abnormal” imaging finding in the asymptomatic population, etc. Injuries that use to be automatically assumed to require surgical intervention 10 years ago are now being called into question. Things like rotator cuff tears, meniscus injuries, lumbar stenosis, etc. are all now being scrutinized much more than a decade ago in the surgical conversation. So a good clinician should be aware of (and more importantly, open to) the idea that their belief system can be called into question and should approach physical medicine with a more humble mentality that we just aren’t always certain. This is better depicted in the infographic below (the Dunning-Kruger effect). In fact, I would argue a patient should be wary of any clinician who acts with an air of certainty when it comes to their particular injury.
-
Create Autonomy. Additionally, I think a good physical therapist is one whose primary mission is to create a robust, resilient and independent patient. We, as a profession, must make it our fundamental mission to teach patients how to be independent participants in their rehabilitation. Any modality, language, or treatment used should fall in line with this concept and any system that fosters dependence must be strongly dissuaded. Essentially, if you think you need me to stay healthy, move well, and enjoy life when we complete our plan of care than I have failed. So what should the role of a good physical therapist be then? We are coaches, guides, and teachers first. I use the analogy of driving on a long road trip to explain this concept to patients. I am your co-pilot and navigator, not your mechanic or chauffeur. I will give you multiple roads and options but ultimately it will be you, the robust resilient patient, that will drive the car and choose the path. If you ask most people what their goal for seeking physical therapy is, the two answers you will receive most often will be “to get out of pain” and often right behind that “to learn how to manage this injury myself.” A good clinician empowers their patients.
-
Treat the person. Finally, a good clinician treats the individual and not the diagnosis. Pain is complex and our old ways of treating pain as purely mechanical (something you can point at on MRI for example) falls woefully short. A good clinician must treat each patient in their entirety, taking account of belief systems, expectations, personality, etc. Two people with the exact same diagnosis may have entirely different presentations so it is paramount to be flexible, adaptive and creative when managing these cases. Programming must be specific to that individual’s goals and symptom response so a good clinician must always be vigilant in avoiding generic exercise prescription and treatment plans. We often tell patients that their experience is unique and to avoid comparing themselves to others (“my neighbor had this and he said he never squatted again!” or “well I shouldn’t complain, it could be much worse…”). At the end of the day, it is the patient living with this pain or limitation and it is the patient in front of us that we must treat
This is by no means an exhaustive list and is likely debatable but after a decade of treating patients and being exposed to various treatment models and theories, this is what I came up with. Hopefully this helps some of you, whether you are a potential future patient or a young clinician and as always, we offer free phone consultations as well as in-person discovery visits where you can come in and see if what we’re all about!